Incorporating both pre-clinical and clinical research components, the Schizophrenia Research Division (SRD) integrates basic, translational, and clinical research focusing on causes and new treatment development in schizophrenia.
Research Goals
- To increase understanding of causes of major mental disorders, most prominently schizophrenia using state-of-the-art neurophysiological and functional brain imaging approaches;
- To integrate across basic and clinical approaches for new paradigm development; and
- To develop new treatment approaches using combined psychopharmacological, cognitive remediation and non-invasive brain imaging-and stimulation-based approaches
PCP/NMDA Model
The research programs of the SRD build upon the PCP/NMDA of schizophrenia, which was first proposed by Dr. Javitt over 25 years ago. Phencyclindine (PCP) and similar agents (e.g. ketamine) induce psychotic symptoms that closely resemble schizophrenia by blocking neurotransmission at N-methyl-D-aspartate (NMDAR)-type glutamate receptors, suggesting that NMDAR dysfunction may play a key role in the pathophysiology of schizophrenia.
Research programs at SRD are dedicated to investigating NMDAR function in both normal and abnormal brain function, and to development of NMDAR-based new treatment approaches for schizophrenia. NMDAR are widely distributed throughout the brain and play a critical role in the both sensory and higher cognitive processing.
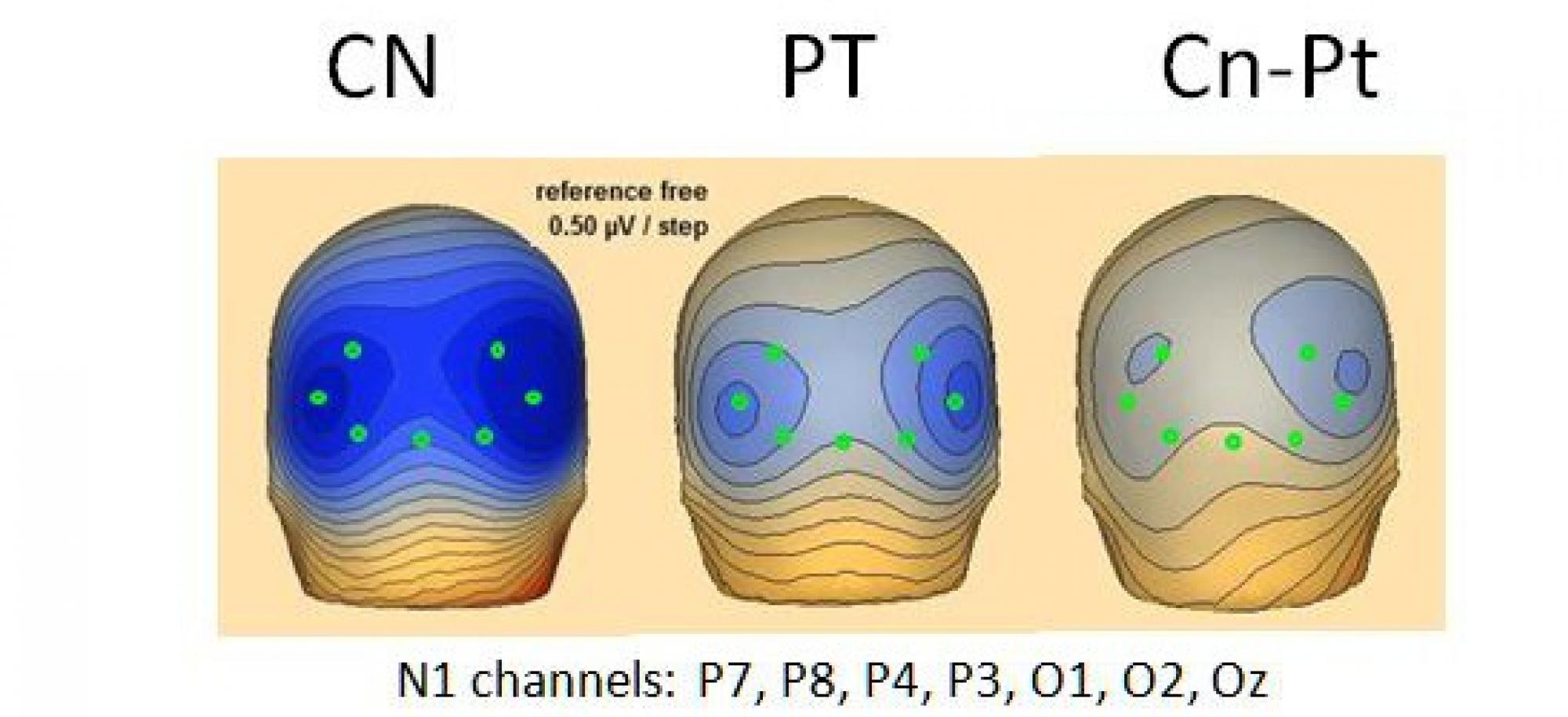
As a result, NMDAR play a critical role in the generation of mismatch negativity (MMN), a biomarker for NMDAR dysfunction that has emerged as a leading predictor of conversion to schizophrenia among individuals at clinical high risk.
Treatment projects within the SRD have demonstrated beneficial effects of several NMDAR-based treatments, including glycine and D-serine, which serve as endogenous modulators of the NMDAR complex.
Research Mission
Schizophrenia is a major mental disorder affecting approximately one percent of the population worldwide. Onset is typically in the 2nd-3rd decade of life with persistent disability thereafter. In addition to the personal consequences of the disease, annual costs of schizophrenia exceed $63 billion in lost wages, disability payments and costs of hospitalization.
Symptoms of schizophrenia are typically divided into positive symptoms such as paranoia or hallucinations; negative symptoms such as apathy, anhedonia, and motor retardation; and cognitive symptoms such as disorientation, disorganized thoughts, and disordered speech.
In addition, patients with schizophrenia typically show a significant decline in cognitive function during the years immediately surrounding illness onset, leading to a decline equivalent to approximately 20 IQ points.
These deficits persist throughout the lifetime of the illness. Although positive symptoms typically respond well to present medications, negative symptoms and cognitive deficits persist and contribute disproportionately to impaired outcome.
The SRD focuses on the development of new treatment approaches to prevent progression of negative symptoms and cognitive deficits early in the course of the disorder, and remediation of deficits in individuals with established deficits.
Recent studies have demonstrated significant reduction in prodromal negative symptoms in at-risk individuals using the NMDAR agonist D-serine, along with reversal of neurophysiological deficits such as MMN in individuals with established schizophrenia.
Other studies have demonstrated sensory-based impairments in functions such as auditory/face emotion recognition and reading ability, which contribute directly to educational and employment difficulties in schizophrenia.
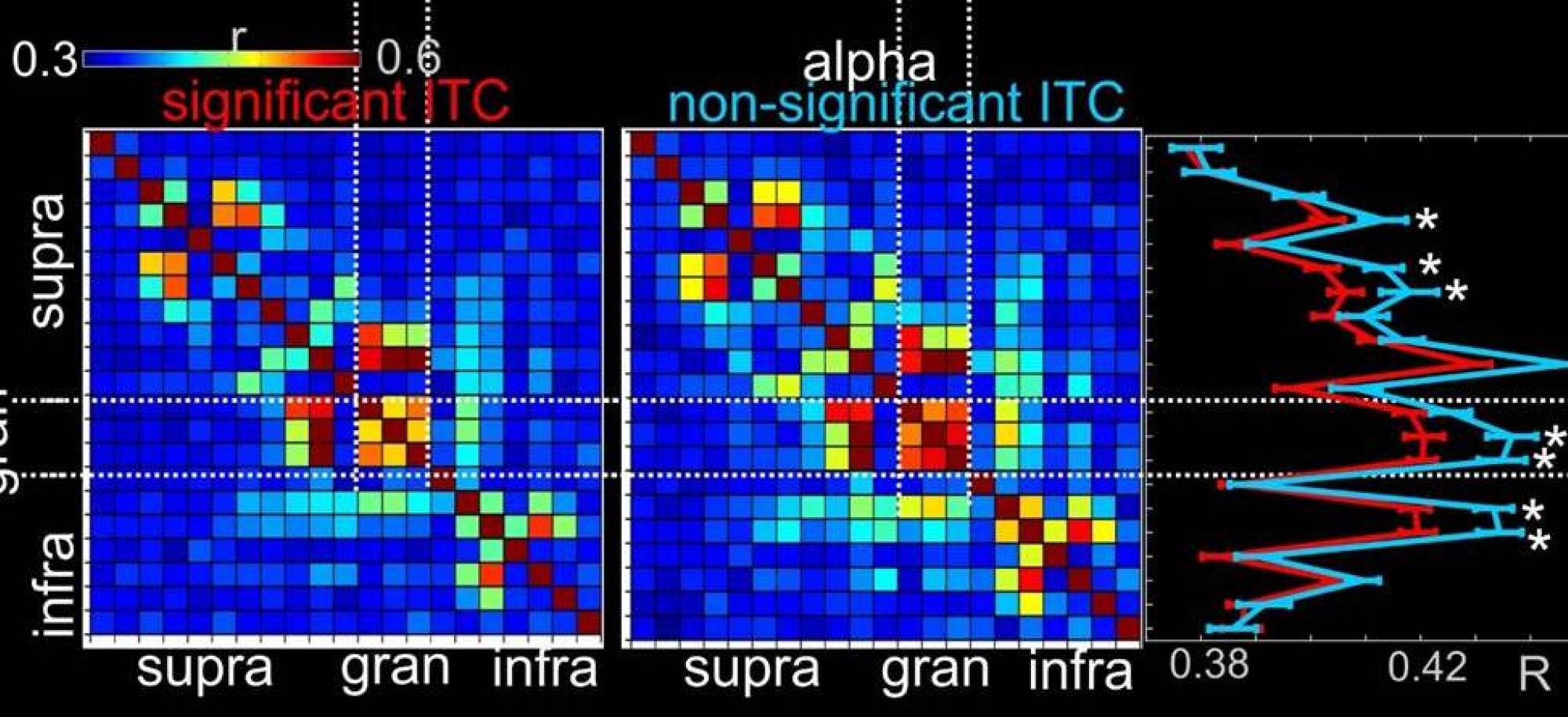
At present, mechanisms underlying cognitive deficits in schizophrenia remain incompletely understood. The SRD conducts parallel studies of cognition in patients, healthy volunteers, and animal models as a mechanism for gaining novel insights into brain-based impairments in cognition in schizophrenia.